Difficulties After Experiencing A Traumatic Brain Injury
- Admin

- May 31, 2023
- 6 min read
What Is a Traumatic Brain Injury (TBI)?
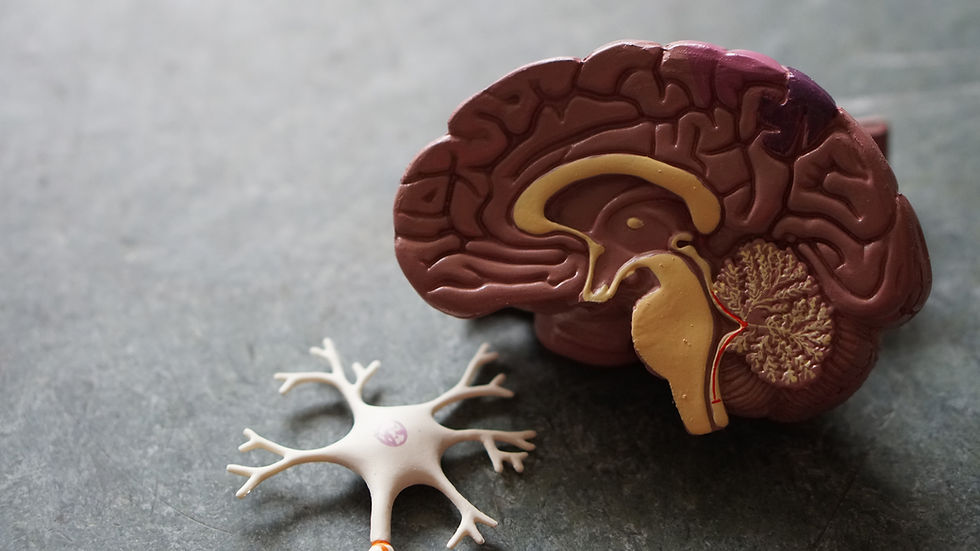
A TBI is linked to various psychiatric and neurobehavioral complications due to severe brain injury (Howlett, Nelson, & Stein, 2022). Such injuries can look like an extreme blow or jolt to the head or can be a penetrating assault to the brain. A TBI can be seen in individuals who have served in the military, professional athletes, those working in highly laborious environments who deal with heavy and dangerous equipment, or anyone involved in serious accidents. It is also reported that some newborns may also suffer from a TBI during childbirth as injuries may occur due to birthing complications, such as the head getting stuck in the birth canal (Poinsett, 2022). Although a TBI is not something that can be predicted it is important to understand that it is a major cause of long-term complications that not only affect those with a TBI directly but also others that interact with them for example coworkers, friends, and family.
To have an understanding of how a TBI impacts those who suffer from it and others that interact with them we will explore how it manifests in various challenges, such as cognitive, physical, and behavioural.
What Are the Cognitive Challenges of A TBI?
A TBI could impair a person’s memory creating challenges in either long-term or short-term memory. If a person is experiencing impairments with their overall memory it would mean that the location of the injury took place in either the hippocampus, the neocortex, and/or the amygdala as these are all areas in control of explicit memories. The basal ganglia and cerebellum are in control of implicit memories, including motor skills, and if these areas are severely injured complications with walking, running, standing, etc., could arise (Reichelt, 2022). It has also been found that challenges in sustained attention and reaction time are variables caused by a TBI (Stocchetti & Zanier, 2016). Challenges with sustained attention can look like individuals who struggle to stay focused on a particular activity for prolonged periods of time which can make working efficiently very difficult, which is commonly found in those who suffer from a TBI. Reaction time is defined as the measure of how fast an internal organism reacts to a stimulus; for instance, someone’s ability to catch a ball that is tossed to them without having to think about the action. Both of these cognitive complications may make the individual’s overall perception steadily decline.
What Are the Physical Challenges of A TBI?
A TBI can create complications for an individual’s overall motor control, which could impact their ability to perform a task without assistance. In some occurrences of severe immobilization, individuals may require consistent care and/or long-term hospitalization, thus making certain aspects of the recovery journey long and laborious. For example, peri-articular calcification, which is excessive swelling around joints, and impaired bladder control may result in extreme handicap and the inability to return to a typical able-bodied life when those with a TBI are hospitalized (Stocchetti & Zanier, 2016).
What Are the Behavioral Challenges of A TBI?
As we have explored how impactful a TBI is on an individual’s cognitive and physical abilities it is important to touch on the behavioral implications as well. According to Taylor and colleagues (2001), there are more adverse effects on an individual’s behavioral abilities compared to their physical and cognitive, more specifically in children. Children who experience severe TBI typically display greater challenges than children with mild to no TBI. These challenges would include increased irritability, confusion, and aggression (Taylor et al., 2001). Children with severe behavioral complications caused by a TBI may exhibit poor communication skills that may make verbalizing their needs very difficult. This could correlate with the cognitive barrier between short-term and long-term memory because the individual may not be able to remember what it is they need, but also how to verbalize it so others can understand them. Due to these behavioral hardships, the individual may develop behavioral disorders, such as depression and anxiety.
Family Member with A TBI
It is reported that family members of an individual who suffers from TBI experience higher levels of psychological distress compared to families who do not have a member with a TBI. However, this is not the case universally as many families are able to cope well with such a change (Gouick & Gentleman, 2004). One of the more stressful elements, for both the individual with a TBI and the family, seems to be the individual's reintegration into society after leaving hospital care because of the added anxiety that comes along with the process. When having a family member who suffers from a TBI extreme changes in their home life should be accommodated once dispatched from hospitalization. These changes could include building ramps if the individual with a TBI is in a wheelchair or crutches, door openers, and widening doors may need to be accounted for in order to make getting around the home as effortless as possible. Furthermore, when having a partner who suffers from a TBI the individual may feel a great deal of disconnect from them due to extreme changes in a variety of ways. These would include the loss of sexual intimacy, overall communication, and declining financial and/or parenting support (Gouick & Gentleman, 2004). When a child is a family member with a TBI a host of worries may be present that are exclusive to their parental figures or caregivers. Such as worries regarding their future and what it could look like, how their TBI will impact their social life, and whether it will be a permanent complication.
Children Raised by A Parent With TBI
Although there has been research conducted on adults and children who suffer from a TBI and the challenges they face, there has been minimal research regarding the effects of being parented by an individual with a TBI. It is widely accounted for that when a child is the one recovering from a TBI there are a host of challenges that affect the entire foundation of the family. However, with little research considering how a child copes when a parent is the one with a TBI, different questions could be explored. Questions such as, ‘Does the child have a support system?’, ‘How does this impact the child’s development?’, ‘Would there be implications on the child-parent relationship?’, and so many more. Opening up the conversation regarding what it is like for the child of a parent or caregiver with a TBI is extremely important to ensure proper research is investigated. We can assume that because of the physical, cognitive, and behavioral attributes previously shared, it can be difficult for the child to recognize their parent and feel wholly comfortable with them as they did before their injury that is if the child had a bond with the parent/caregiver before the injury. Thus, the child may not acknowledge that their parent/caregiver suffers from a TBI because it is.
In Conclusion…
A TBI can be a serious condition that may impact everyone involved with the individual suffering from it. Hopefully understanding the different challenges behind it, such as the physical, behavioral, and cognitive difficulties, makes it easier to empathize with those who experience a TBI and those who interact with an individual with a TBI. If you are someone who interacts with an individual with a TBI, whether that be a parent, a child of a parent, a coworker, or a friend, ensuring you have a reliable support system of your own is just as crucial. We have a list of professional therapists here at RMTC who will be happy to be a part of your support system whenever you feel comfortable! Contact us at (226) 894-4112 or by email at admin@relationshipmatterstherapy.com.
Sources:
Gouick, J., & Gentleman, D. (2004). The emotional and behavioural consequences of Traumatic Brain Injury. Trauma, 6(4), 285–292. https://doi.org/10.1191/1460408604ta323oa
Howlett, J. R., Nelson, L. D., & Stein, M. B. (2022). Mental health consequences of traumatic brain injury. Biological Psychiatry, 91(5), 413–420. https://doi.org/10.1016/j.biopsych.2021.09.024
Poinsett, P. M. (2022, March 11). Infant brain damage symptoms: Signs to watch for. Cerebral Palsy Guidance. Retrieved March 1, 2023, from https://www.cerebralpalsyguidance.com/birth-injury/infant-brain-damage/symptoms/#:~:text=Infant%20brain%20damage%20can%20result,childbirth%20because%20of%20birth%20injuries.
Reichelt, A. (2022, August 4). We're capable of infinite memory, but where in the brain is it stored, and what parts help retrieve it? The Conversation. Retrieved February 15, 2023, from https://theconversation.com/were-capable-of-infinite-memory-but-where-in-the-brain-is-it-stored-and-what-parts-help-retrieve-it-63386
Stocchetti, N., & Zanier, E. R. (2016). Chronic impact of traumatic brain injury on outcome and quality of life: A narrative review. Critical Care, 20(1). https://doi.org/10.1186/s13054-016-1318-1
Taylor, H. G., Yeates, K. O., Wade, S. L., Drotar, D., Stancin, T., & Burant, C. (2001). Bidirectional child–family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society, 7(6), 755-767.



